What is Medical Retina?
Retina is the photosensitive layer of the nerve cells lining the inside of the eye. It is affected in some hereditary disorders, diabetes, hypertension, blood disorders, injuries, vascular occlusions, aging and lot of other conditions. Cases with retinal disorders feel painless rapid loss of vision. Grewal Eye Institute is fully equipped to diagnose and manage all kind of retinal disorders. We are equipped to manage patients with diabetic retinopathy, diabetic maculopathy, branch retinal vein occlusion (BRVO) and central retinal vein occlusion (CRVO), choroidal neovascular membranes (CNVM), eales disease and retinal vasculitis, retinal breaks and lattice degeneration with holes, Central serous chorioretinopathy (CSCR,) proliferative vitreo-retinopathies and many other retinal disorders. Digital fundus fluorescein angiography (STEREO), visual fields and laser are available for management of these cases. A Diode laser is available for anterior and posterior segment with endo photo coagulation attachment. The IRIS diode laser was the first such unit installed in our country. A double frequency Yag Laser (532 green) has been added recently.
About Diabetic Retinopathy
Diabetic Retinopathy, a complication of diabetes, is caused by changes in the blood vessels of the retina, the light sensing nerve layer at the back of the eye. These damaged blood vessels leak fluid or blood, and develop fragile brush like branches and scar tissue. The images which the retina sends to the brain become blurred, distorted or partially blocked.
Diabetic Retinopathy is the leading cause of blindness among adults in our country. This increase has been due to the improved life expectancy of the diabetic patients. People with untreated diabetes are said to be twenty five times more prone to blindness than the general population. However, with improved methods of diagnosis and treatment, only a small percentage of those who develop retinopathy experience serious problems with vision.
FAQs about Diabetic Retinopathy
Who gets Diabetic Retinopathy?
Obviously, only diabetics get diabetic retinopathy. The risk of developing diabetic retinopathy increases with the duration of diabetes, about 80% of people with diabetes of more than fifteen years, have some damage to the blood vessels of their retina. Uncontrolled diabetes, fluctuating blood sugar levels, hypertension (high blood pressure), long duration of diabetes, high blood cholesterol and diabetic kidney, predispose a diabetic to develop changes in retina. Pregnancy and high blood pressure may aggravate diabetic retinopathy. It is very important to know that the retina is affected when the blood sugar level comes down. Therefore, it is very important, not to panic when the blood sugar goes high. Once should take time to bring it down. Fluctuations in blood sugar levels are to be avoided at any cost. Diabetic retinopathy occurs at a younger age in juvenile diabetics, the one who have been diagnosed with the condition during their childhood or teenage years.
About Diabetes Mellitus
A small soft globular organ by the name of pancreas secrets a hormone known by the name of insulin which is necessary in the body to burn sugars. The lack of absence of this hormone leads to the known signs and symptoms of diabetes mellitus. The only treatment available is to supplement this insulin. The tablets stimulate the production of insulin by the patient's pancreas. If pancreas fail to produce insulin, it needs to be supplemented from external sources through injections. A diabetic remains so for whole of his life. An adequate control of diabetes calls for a balance of three things : 1. Diet 2. Drug 3. Exercise (Physical Activity). In case of increased levels of blood sugar a diabetic should cut down on the diet (decrease the calorie load on body) and increase the drug and also increase physical exercise (to burn more calories). A diabetic who understands the interplay of these factors is at a great advantage to control his or her diabetes.
Type of Diabetic Retinopathy
There are two types or stages of diabetic retinopathy .
Background retinopathy is an early state of diabetic retinopathy. In this stage, fine blood vessels within the retina become narrowed or obstructed while others enlarge to form balloon-like sacs. These altered vessels leak blood and fluid, causing the retina to swell or form deposits called exudates. Sight is usually not seriously affected. It can, however lead to more advanced sight-threatening stages, and for this reason is considered a warning sign.
In some cases, the leaking fluid collects in the macula, the central part of the retina which is responsible for detailed vision, such as reading. This problem is called macular oedema or diabetic maculopathy. Reading and close work may become more difficult because of this condition. . vessels leak blood and fluid, causing the retina to swell or form deposits called exudates. Sight is usually not seriously affected. It can, however lead to more advanced sight-threatening stages, and for this reason is considered a warning sign. In some cases, the leaking fluid collects in the macula, the central part of the retina which is responsible for detailed vision, such as reading. This problem is called macular oedema or diabetic maculopathy. Reading and close work may become more difficult because of this condition.
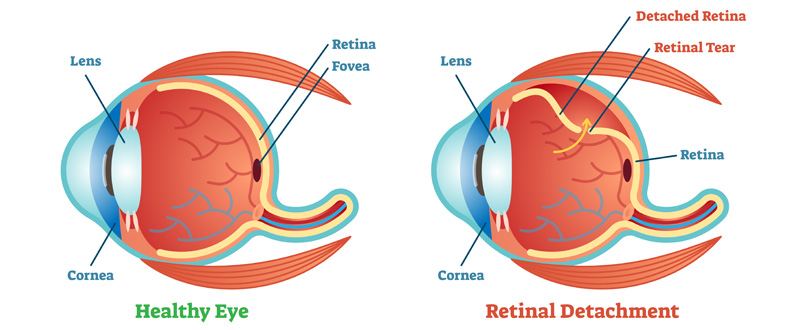
Proliferative retinopathy is an advanced stage. It describes the changes that occur when new, abnormal blood vessels begin to grow on the surface of the retina or the optic nerve. These new blood vessels, called neovascularisation, have weaker walls and may rupture and bleed into the vitreous, the clear gel like substance that fills the centre of the eye. This leaking blood can cloud the vitreous and partially block the light through the pupil towards the retina, causing blurred and distorted images. These abnormal blood vessels frequently grow scar like tissue with them which may pull the retina away from its normal position at the back of the eye (detached retina). Abnormal blood vessels may also grow around the pupil causing glaucoma by increasing pressure within the eye. Proliferative diabetic retinopathy is the most serious form of diabetic retinal disease. It affects up to 20% of diabetics and can cause severe loss of sight, including blindness.
Causes and Symptoms
The cause of diabetic retinopathy is not completely understood. However, it is known that diabetes damages small blood vessels in various parts of the body. The damage to the tiny blood vessels in the retina occurs when the blood sugar levels come down rapidaly. Every fluctuation is thus dangerous.
Diabetic retinopathy is a painless condition. It is not associated with redness or watering or irritation of the eye. One can have background diabetic retinopathy for a long time without any effect on vision. Thus changes in the eye can go unnoticed unless detected by a medical eye examination. Gradual painless blurring of vision may occur if macular oedema is present. A sudden loss of vision can occur if bleeding occurs inside the eye with proliferative retinopathy. This severe form of diabetic retinopathy requires immediate medical attention.
Detection & Diagnosis
A comprehensive medical eye examination and appropriate treatment by an ophthalmologist is the best protection against eye damage due to diabetic retinopathy. Serious retinopathy can be present without symptoms. Therefore, people with diabetes should be aware of the risks of developing visual problems and should have their eyes examined regularly. (Periodic eye examinations are also advised for apparently healthy people above forty years of age, because such examination may help detect the presence of diabetes and other diseases).
To detect diabetic retinopathy, the ophthalmologist conducts a painless examination of the inner part of the eye using an instrument called an ophthalmoscope. The pupil is dilated with special eye drops instilled about an hour before the examination.
If diabetic retinopathy is noted, the ophthalmologist may obtain colour photographs of the retina. Sometimes a specialized technique, called fundus fluorescein angiography (FFA), is used to provide fine details of retinal and other diseases.
To detect diabetic retinopathy, the ophthalmologist conducts a painless examination of the inner part of the eye using an instrument called an ophthalmoscope. The pupil is dilated with special eye drops instilled about an hour before the examination.
If diabetic retinopathy is noted, the ophthalmologist may obtain colour photographs of the retina. Sometimes a specialized technique, called fundus fluorescein angiography (FFA), is used to provide fine details of retinal blood vessels and the leakages from them. First, a fluorescent dye is injected into a vein in the arm. The dye travels through the bloodstream to reach the blood vessels in the retina. Photographs are taken in rapid succession as the dye passes through the retinal blood vessels.Besides diagnosis it forms an important basis to plan the treatment. The arrival of Digital Angiography in the scenario has added an undue advantage to plan the management promptly. This involves real time imaging of the procedure as the dye transmits the vessels.
When diabetic retinopathy is diagnosed, the ophthalmologist considers the patient's age, history, lifestyle and the degree of damage to the retina before deciding whether treatment or further observation of the disease is most appropriate. In many cases treatment is not necessary; in others it is recommended to halt the progress of diabetic retinopathy and improve sight wherever possible.
Call to book an Appointment
+91 9219440775
Hi-Tech Hospital
Giritial, Kashipur
Udham Singh Nagar
Uttarakhand - 244713